O ccupational Therapy Toolkit ™
Patient Handouts and Treatment Guides
for
Adults
Physical Disabilities, Chronic Conditions, and Geriatrics
O ccupational Therapy Toolkit ™
Impairments and Functional Limitations
ADL, IADL, productivity and leisure impairment
Impaired functional mobility
Hemiparesis or hemiplegia of the upper and lower extremities
Spasticity
Impaired postural control and balance
Impaired coordination
Limited activity tolerance and endurance
Impaired sensation
Central post-stroke pain
Language disorders (aphasia, dysarthria, dyspraxia)
Dysphasia
Visual and perceptual impairment
Cognitive impairment
Behavioral disorders (depression, lability, low frustration tolerance, impulsivity)
Bladder and bowel dysfunction
Potential secondary complications may include biomechanical shoulder pain (biceps tendonitis, rotator cuff pathology, adhesive capsulitis, complex regional pain syndrome), edema (upper and lower extremity), pressure ulcers, joint contractures, depression, DVT’s, aspiration pneumonia, seizures, fall risk
Assessments
Assessment of Motor and Process Skills
Chedoke-McMaster Stroke Assessment Scale
Modified Ashworth Scale of Spasticity
Stroke Impact Scale
Occupational Therapy Intervention
ADL, IADL, productivity and leisure training
- Safely incorporate affected extremity with all activities.
- Use compensatory techniques (task modification, one-handed techniques, hand-over-hand guiding, task segmentation, backward chaining).
- Recommend and/or provide adaptive equipment. Rocker knife, inner lip plates, holders for books or playing cards, stabilizing devices for activities that traditionally require two-handed performance (cutting vegetables, cleaning dentures), and keyboards adapted for one-handed computer use.
- Instruct in pacing and energy conservation strategies.
Train in safe and efficient functional mobility (sit-to-stand, bed mobility skills, transfers, standing, ambulation, and wheelchair mobility) during ADL and IADL tasks.
Provide functional posture and balance activities.
- Focus on stability, weight shifting, body awareness, trunk rotation & elongation.
- Have patient turn toward affected side when reaching.
- Set up room so the patient must physically move to their affected side.
- Provide reach-grasp-hold-release activities, in standing and sitting, with and without support.
Provide activities and exercises to uninvolved side to prevent loss of ROM and strength.
Restore function of the upper extremity. Use a variety of remedial approaches according to the needs of the patient.
- Provide early mobilization and positioning.
- Incorporate task-oriented/task specific training.
- Provide opportunities to use and move the arm throughout the day (use of mobile arm support, overhead suspension sling, functional splinting such as wrist cock-up, and dynamic finger extension splints).
- Provide modified constraint-induced movement therapy or constraint-induced movement therapy.
- Instruct an arm and hand strengthening exercise program.
- Cyclic NMES during functional movements and activity.
- Instruct in a functional dynamic orthoses (SaeboFlex, SaeboReach).
- Use cognitive strategies (mirror therapy, mental imagery/practice, action observation).
- Provide sensory re-education intervention.
- Avoid increasing spasticity.
- Encourage use of extremity in functional tasks.
- Provide weight-bearing activities.
- Provide sensory stimulation activities.
- Teach compensatory techniques and safety measures for sensory deficits. Use vision to compensate for sensory loss. Test bath/dish water temperature using the intact extremity or a thermometer. Use a thermal regulation valve to lower water temperature. Avoid using heating pads on impaired extremities. Wear gloves to prevent frostbite. Avoid going barefoot. Wear sunscreen to prevent sunburn. Avoid cuts and burns in kitchen. Use intact hand to handle sharp kitchen utensils. Perform skin checks.
- Prevent or manage hand edema.
- Teach active self-range of motion exercises in elevation.
- Position hand in elevation
- Use retrograde massage.
- Use gentle grade 1-2 mobilizations for the hand and fingers.
- Provide a compression garment.
- Manage spasticity.
- Prevent contractures.
- Provide PROM, SROM and stretching exercises.
- Instruct in positioning in bed, chair and during mobility.
- Select use of splinting to protect hand/wrist. Resting hand splint for flaccid to mild tone, spasticity splint for moderate to high tone. Reassess frequently and discontinue of there is no benefit.
- Post-Botox injections, provide strengthening/FES to antagonists, stretching and splinting
- Prevent or manage shoulder pain.
- Avoid overaggressive therapy and overhead pulleys.
- Mobilize and strengthen the scapula.
- Position arm with cubital fossa facing up, 45º shoulder abduction and comfortable shoulder external rotation.
- Provide firm support devices such as lap trays and arm troughs.
- Range of motion exercises should not move the shoulder beyond 90°of flexion and abduction unless there is upward rotation of the scapula and external rotation of the humeral head.li>
- o Manage acquired orthopedic conditions (biceps tendonitis, impingement syndrome, adhesive capsulitis, rotator cuff pathologies, CRPS).
- Use functional electrical stimulation (FES) for shoulder subluxation.
Instruct patient and caregivers in care of the affected extremity.
- Prevent and control of edema.
- Teach passive ROM exercises.
- Teach self-ROM exercises.
- Protect and support the affected arm during bed mobility, transfers and ambulation using slings, a pocket, or hand hold and during wheelchair use by using a hemi tray or arm trough.
- Teach proper positioning in bed, chair and wheelchair.
- Instruct in care and use of positioning splints.
Teach compensatory strategies for perceptual deficits.
Provide cognitive retraining and train in the use of compensatory strategies.
Provide education about fall risk and prevention strategies.
Community reintegration
- Complete a comprehensive, performance-based home assessment. Recommend and/or provide modifications, adaptive equipment and/or assistive technology.
- Encourage leisure and social participation.
- Address ability to drive safely. Provide referral to driving rehab specialist and/or explore alternative transportation options.
- Recommend vocational rehabilitation strategies to assist with return to work if appropriate.
Teach strategies to incorporate wellness and health management routines into daily activities.
Educate patient and caregivers about stroke, the availability of community resources. and support groups. Provide educational materials about stress management, coping strategies, and occupational balance.
Patient and Caregiver Education Handouts
Edema (Swelling) Control of the Arm(s)
Edema (Swelling) Control of the Leg(s)
In and Out of Bed - Toward Your Weaker Left Side
In and Out of Bed - Toward Your Weaker Right Side
Position in Bed - Left Side Weakness
Position in Bed - Right Side Weakness
Position Your Arm - Left Side Weakness
Position Your Arm - Right Side Weakness
Protect the Arm - Left Side Weakness
Protect the Arm - Right Side Weakness
Splint/Brace Instructions
Stress Management
Tips to Conserve Energy
Using a Front Wheel Walker (2 wheels)
Wheelchair Safety
Patient and Caregiver Exercise Handouts
Balance Exercises - Sitting and Standing
Fine Motor Strengthening and Coordination Activities
Gross Motor Tasks
Level 1 Activities - Help Your Weaker Arm Move
Level 2 Activities - Use Your Weaker Arm to Passively Hold
Level 3 Activities - Use Your Weaker Arm to Actively Move and Hold
Level 4 Activities - Use Your Weaker Arm with Gross Motor
Level 5 Activities - Use Your Weaker Arm with Fine Motor
Passive Range of Motion - One Side Weakness
Posture Exercises
Putty Exercises
Scapular Mobility and Strength Exercises
Self Range of Motion
Upper Body Active Range of Motion
Upper Body Exercises - Dumbbells
Upper Body Exercises - Holding a Ball
Upper Body Strength Activities
Use Your Arm to Actively Move and Hold
Use Your Arm to Hold Passively
Use Your Arm with Assisted Guiding
Use Your Arm with Gross Motor Activities
Use Your Arm with Self-Guiding
Weight Bearing Exercises
Additional Treatment Guides
Activities of Daily Living
Apraxia
Balance
Cognition
Depression
Fall Risk Assessment and Prevention
Functional Mobility
Handwriting
Health Management
Home Safety and Modification
Therapeutic Exercise
Visual Skills
Wheelchair Seating, Positioning, and Mobility
O ccupational Therapy Toolkit ™
ADLs and IADLs
Bathing and Showering
Clothing Care
Communication Management
Community Mobility
Dressing
Driving
Feeding, Eating and Swallowing
Financial and Mail Management
Functional Communication
Functional Mobility
Grooming and Hygiene
Health Management
Home and Yard Maintenance
Leisure Activities
Meal Preparation and Cleanup
Medication Management
Rest and Sleep
Safety and Emergency Preparedness and Response
Sexual Expression and Activity
Shopping
Toileting and Toilet Hygiene
Work and Industry
Balance
Cognition
Fall Prevention and Fall Risk Reduction
Handwriting
Home Safety and Modification
Therapeutic Exercise
Visual Skills
Wheelchair Seating, Positioning, and Mobility
Alzheimer’s Disease and Related Dementias - Early Stage
Alzheimer’s Disease and Related Dementias - Mid Stage
Alzheimer’s Disease and Related Dementias - Late Stage
Amputation of the Lower Limb
Amputation of the Upper Limb
Amyotrophic Lateral Sclerosis (ALS)
Ankylosing Spondylitis
Anxiety Disorder
Arthritis
Biceps Tendinitis
Breast Cancer
Burn Injury
Cancer
Cardiac Disease
Cardiac Surgery
Carpal Tunnel Syndrome - Conservative
Carpal Tunnel Syndrome - Postoperative
Cervical Stenosis, Myelopathy and Radiculopathy
Cervical Spine Surgery
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Pain Syndrome
Complex Regional Pain Syndrome
Cubital Tunnel Syndrome - Conservative
Cubital Tunnel Syndrome - Postoperative
Depression
De Quervain's Syndrome Diabetes
Dizziness
Emphysema (see Chronic Obstructive Pulmonary Disease)
Epicondylitis
Fibromyalgia (see Chronic Pain Syndrome)
Fracture of the Elbow
Fracture of the Hip
Fracture of the Shoulder
Fracture of the Wrist
Frailty and Debility
Frozen Shoulder (Adhesive Capsulitis)
Golfer’s Elbow (see Epicondylitis)
Guillain-Barré Syndrome
Huntington's Disease
Joint Contractures
Kidney Disease
Low Back Pain (see Chronic Pain Syndrome)
Low Vision and Blindness
Lumbar Stenosis
Lumbar Spine Surgery
Lupus (Systemic Lupus Erythematosus)
Lymphedema
Medically Complex and Critically Ill in the ICU
Mild Cognitive Impairment
Multiple Sclerosis
Myasthenia Gravis - Generalized
Myocardial Infarction
Obesity and Bariatric Care
Osteoporosis
Palliative Care and Hospice
Parkinson's Disease - Early Stage
Parkinson's Disease - Mid Stage
Parkinson's Disease - Late Stage
Peripheral Neuropathy
Post-Acute Sequela of COVID- (PASC)
Post-Polio Syndrome
Pressure Ulcers
Reverse Total Shoulder Arthroplasty
Rotator Cuff Arthroscopic Repair
Rotator Cuff Pathology
Scleroderma (Systemic Sclerosis)
Spinal Cord Injury Paraplegia T-S
Spinal Cord Injury Tetraplegia/Quadriplegia C
Stroke
Tennis Elbow (see Epicondylitis)
Total Hip Replacement (Arthoplasty)
Total Knee Replacement (Arthoplasty)
Total Shoulder Arthroplasty and Hemiarthroplasty
Traumatic Brain Injury - Mild (mTBI)
Traumatic Brain Injury - Rancho Levels I, II, III
Traumatic Brain Injury - Rancho Levels IV, V, VI
Traumatic Brain Injury - Rancho Levels VII, VIII, IX, X
Trigger Finger/Thumb (Stenosing Tenosynovitis)
Urinary Incontinence
Vertebral Compression Fracture
Adaptive Equipment
Adaptive Equipment for Dressing
Adaptive Equipment for Eating
Adaptive Equipment for Grooming and Mouth Care
Adaptive Equipment for Meal Prep
Adaptive Equipment for Mobility
Adaptive Equipment for Moving in Bed
Adaptive Equipment for Transfers
Adaptive Equipment for Using the Bathroom
Adaptive Equipment for Walking
Using a Rollator (3 or 4 wheels)
Using a Standard Walker (no wheels)
Walk with a Cane on the Stronger, Left Side
Walk with a Cane on the Stronger, Right Side
Walk with a Standard Walker - Full Weight Bearing
Walk with a Standard Walker - Non-Weight Bearing
Walk with a Standard Walker - Partial Weight Bearing
Walk with a Standard Walker - Toe-Touch Weight Bearing
Walk with a Standard Walker - Weight Bearing as Tolerated
Walk with a Wheeled Walker - Full Weight Bearing
Walk with a Wheeled Walker - Weight Bearing as Tolerated
How to Install Grab Bars - Faucet on the Left
How to Install Grab Bars - Faucet on the Right
Transfer to Shower Chair (back up, turn left)
Transfer to Shower Chair (back up, turn right)
Transfer to Shower Chair (left leg, right leg, sit)
Transfer to Shower Chair (right leg, left leg, sit)
Transfer to Shower Chair (left leg, sit, right leg)
Transfer to Shower Chair (right leg, sit, left leg)
Transfer to Tub Bench - After Hip Surgery (back up, turn left)
Transfer to Tub Bench - After Hip Surgery (back up, turn right)
Transfer to Tub Bench (back up, turn left)
Transfer to Tub Bench (back up, turn right)
Transfer Wheelchair to Tub Bench - Move to the Left
Transfer Wheelchair to Tub Bench - Move to the Right
In and Out of Bed - Toward Your Left Side
In and Out of Bed - Toward Your Right Side
In and Out of Bed - Toward Your Left Side After Hip Surgery
In and Out of Bed - Toward Your Right Side After Hip Surgery
In and Out of Bed - Toward Your Left Side Log Rolling
In and Out of Bed - Toward Your Right Side Log Rolling
In and Out of Bed - Toward Your Weaker Left Side
In and Out of Bed - Toward Your Weaker Right Side
In and Out of Bed with Help - Toward Their Left Side
In and Out of Bed with Help - Toward Their Right Side
Move From One Side of the Bed to the Other
Move Up in Bed
Roll onto Your Left Side
Roll onto Your Right Side
Put On and Take Off a T-shirt - Arm-Head-Arm
Put On and Take Off a T-shirt - Head-Arm-Arm
Put On and Take Off a T-shirt Using a Dressing Stick
Put On and Take Off an Ankle-Foot Brace - Method 1 - Left Leg
Put On and Take Off an Ankle-Foot Brace - Method 1 - Right Leg
Put On and Take Off an Ankle-Foot Brace - Method 2 - Left Leg
Put On and Take Off an Ankle-Foot Brace - Method 2 - Right Leg
Put On and Take Off an Open Front Shirt - One Shoulder Drape
Put On and Take Off an Open Front Shirt - Two Shoulder Drape
Put On and Take Off an Open Front Shirt Using a Dressing Stick
Put On and Take Off Pants - Method 1
Put On and Take Off Pants - Method 2
Put On and Take Off Pants, Socks, and Shoes Lying Down
Put On and Take Off Pants, Socks, and Shoes Using a Stool
Put On and Take Off Pants Using a Dressing Stick or Reacher
Put On and Take Off Socks and Shoes Using Dressing Tools
Put On and Take Off Support Stockings
Using a Buttonhook
Put On a T-shirt with One Hand - Right Side Weakness
Put On an Open Front Shirt with One Hand - Left Side Weakness
Put On an Open Front Shirt with One Hand - Right Side Weakness
Put On and Take Off a Bra with One Hand - Left Side Weakness
Put On and Take Off a Bra with One Hand - Right Side Weakness
Put On Pants with One Hand - Left Side Weakness
Put On Pants with One Hand - Right Side Weakness
Put On Socks and Shoes with One Hand - Left Side Weakness
Put On Socks and Shoes with One Hand - Right Side Weakness
Take Off a T-shirt with One Hand - Left Side Weakness
Take Off a T-shirt with One Hand - Right Side Weakness
Take Off an Open Front Shirt One Hand - Left Side Weakness
Take Off an Open Front Shirt One Hand - Right Side Weakness
Take Off Pants with One Hand - Left Side Weakness
Take Off Pants with One Hand - Right Side Weakness
Tie Shoes with One Hand - Left Side Weakness
Tie Shoes with One Hand - Right Side Weakness
Tips for Making and Keeping Health Care Visits
Manage Kitchen Tasks with a Wheelchair
Meal Prep with One Hand
Down Steps with a Rail Using a Cane
Down Steps with a Rail Using a Closed Walker
Down Steps with a Rail Using an Open Walker
Down Steps without a Rail Using a Cane
Up a Curb or Single Step Using a Walker
Up Steps with a Rail Using a Cane
Up Steps with a Rail Using a Closed Walker
Up Steps with a Rail Using an Open Walker
Up Steps without a Rail Using a Cane
Toileting Options - Therapist Resource
Using a Urinal
Get Down On the Floor
Get Up From the Floor
Sit-Pivot Transfer - Move to the Left
Sit-Pivot Transfer - Move to the Right
Sit-Pivot Transfer with Help - Move to Their Left
Sit-Pivot Transfer with Help - Move to Their Right
Sitting Down from a Rollator
Sitting Down from a Walker
Sitting Down After Hip Surgery
Standing Up to a Rollator
Standing Up to a Walker
Standing Up with Help
Stand-Pivot Transfer with Help - Move to Their Left
Stand-Pivot Transfer with Help - Move to Their Right
Transfer Board - Move to the Left
Transfer Board - Move to the Right
Wheelchair Positioning
Wheelchair Safety
Amputation
Care of the Prosthesis and Upper Limb Coverings
Care of Your Residual Limb
Phantom Limb Pain
Position Your Residual Limb - AKA
Position Your Residual Limb - BKA
Breathing Distress Control
Cardiac Precautions for Exercise
Controlled Cough
Daily Tasks after Open Heart Surgery - Standard Precautions
Deep (Diaphragmatic) Breathing
Fatigue Journal - Mental Activity
Fatigue Journal - Physical Task
How to Check Your Heart Rate
Postural Drainage Positions
Pursed Lip Breathing
Safety Tips for Using Home Oxygen
Sternal Precautions - Standard
Tips to Conserve Energy
Tips to Conserve Energy with Meal and Home Tasks
Tips to Conserve Energy with Self Care Activities
Functional Cognitive Activities
Tips to Improve Attention
Tips to Improve Figure Ground
Tips to Improve Form Constancy
Tips to Improve Left Side Awareness
Tips to Improve Memory
Tips to Improve Memory - External Memory Aids
Tips to Improve Memory - Internal Memory Aids
Tips to Improve Motor-Planning
Tips to Improve Right Side Awareness
Tips to Improve Thinking Skills
Tips to Improve Vision
Tips to Improve Visual-Motor Integration
Tips to Improve Visual Spatial Relations
Body Mechanics - Lifting Lightweight Objects
Body Mechanics - Lifting Medium Weight Objects
Body Mechanics - Lifting Heavy Objects
Body Mechanics - Limit Bending, Twisting, and Reaching
Computer Workstations
Contributing Factors for Workplace Injuries
Joint Protection and Energy Conservation for Wheelchair Users
Joint Protection for Arthritis
Handwriting - Cursive Lower Case Letters
Handwriting - Pangrams
Handwriting - Print Component Exercises
Handwriting - Print Lower Case Letters
Writing Tips for Parkinson’s
Low Vision - Functional Reading
Low Vision - Functional Vision
Low Vision - Improve Your Other Senses
Low Vision - Kitchen Tasks
Low Vision - Label and Mark Items
Low Vision - Leisure
Low Vision - Lighting
Low Vision - Medication
Low Vision - Money
Low Vision - Moving Around
Low Vision - Reading, Writing, Phone Use
Low Vision - Reduce Glare
Low Vision - Safety
Low Vision - Use Contrast
Position in Bed - Left Side Weakness
Position in Bed - Right Side Weakness
Position Your Arm - Left Side Weakness
Position Your Arm - Right Side Weakness
Protect the Arm - Left Side Weakness
Protect the Arm - Right Side Weakness
Tips to Manage Action Tremors
Arm Measurement for Lymphedema
Checking Your Skin
Desensitization
Edema (Swelling) Control of the Arm(s)
Edema (Swelling) Control of the Leg(s)
Good Sleep Habits
Leg Measurement for Lymphedema
Leisure Activities
Pain Journal
Position in Bed to Reduce Pressure
Pressure Relief When Sitting
Scar Massage
SMART Goals
SMART Goals - Action Plan
Stress Management
Stress Management - Relaxation Tools
Stress Management - Stress Journal
Tips to Prevent Lower Body Lymphedema
Tips to Prevent Upper Body Lymphedema
Using Cold for Pain Relief
Using Heat for Pain Relief
Daily Tasks after Neck (Cervical) Surgery
Daily Tasks after Shoulder Surgery
Spinal Surgery Precautions
Splint/Brace Instructions
Total Hip Precautions - Anterior Approach
Total Hip Precautions - Posterior Approach
Don’t Let a Fall Get You Down - Post-Fall Survey
Fall Triggers and Tips to Prevent Falls
Foot Care and Foot Safety
Home Safety and Performance Assessment
Balance Core Exercises
Balance Exercises - Sitting
Balance Exercises - Standing
Core Exercise Guidelines
Core Exercises - Back Muscles
Core Exercises - Pelvic Muscles
Core Exercises - Stomach Muscles
Core Exercises - Seated
Exercise Ball Guidelines
Exercise Ball - Back Muscles
Exercise Ball - Pelvic Muscles
Exercise Ball - Stomach Muscles
De Quervain’s Exercises - Left
De Quervain’s Exercises - Right
Elbow Stretches for Below Elbow Amputation
Epicondylitis Exercises - Left
Epicondylitis Exercises -Right
Exercise Tips for Amyotrophic Lateral Sclerosis
Exercise Tips for Arthritis
Exercise Tips for Diabetes
Exercise Tips for Guillain-Barré Syndrome
Exercise Tips for Multiple Sclerosis
Exercise Tips for Myasthenia Gravis
Exercise Tips for Orthopedic Conditions
Exercise Tips for Post-Polio Syndrome
Exercise Tips for Renal Conditions
General Exercise Tips
Mastectomy Exercises
Osteoporosis Extension Exercises
Parkinson’s Exercises
Pelvic Floor (Kegel) Exercise
Pulmonary Exercises
Elbow, Forearm and Wrist Strength Exercises
Elbow, Forearm and Wrist Stretches
Elbow, Wrist, and Hand Active ROM (shoulder surgery)
Forearm and Wrist Active Range of Motion
Forearm and Wrist Strength Exercises
Forearm and Wrist Stretches
Finger and Thumb Strength Exercises - Left
Finger and Thumb Strength Exercises - Right
Finger and Thumb Stretches and Active Range of Motion - Left
Finger and Thumb Stretches and Active Range of Motion - Right
Finger Active Range of Motion - Left
Finger Active Range of Motion - Right
Finger Passive Range of Motion - Left
Finger Passive Range of Motion - Right
Median Nerve Glides for Carpal Tunnel Syndrome
Putty Exercises
Tendon Glides
Thumb Active Range of Motion - Left
Thumb Active Range of Motion - Right
Thumb Passive Range of Motion - Left
Thumb Passive Range of Motion - Right
Ankle and Foot Isometric Exercises
Ankle and Foot Strength Exercises
Ankle and Foot Stretches
Hip and Knee Exercises - Lying
Hip and Knee Exercises - Seated
Hip and Knee Exercises - Standing
Low Back Stretches
Resistance Band Exercises - Legs
Self Range of Motion - Lower Body
Thigh Stretches
Stretch Break
Walking Guidelines
Walking Warm-Up Exercises
Neck Active Range of Motion
Neck Isometric Exercises
Neck Strength Exercises
Neck Stretches
Rotator Cuff Active Range of Motion - Right
Rotator Cuff Protection and Gentle Stretching - Left
Rotator Cuff Protection and Gentle Stretching - Right
Rotator Cuff Strengthening Exercises - Left
Rotator Cuff Strengthening Exercises - Right
Shoulder Active Range of Motion - Left
Shoulder Active Range of Motion - Right
Shoulder and Hand Active Range of Motion
Shoulder Cane Exercises - Supine - Left
Shoulder Cane Exercises - Supine - Right
Shoulder Cane Exercises – Standing
Shoulder Dumbbell Exercises
Shoulder, Elbow, and Hand Active Range of Motion
Shoulder Isometric Exercises - Seated - Left
Shoulder Isometric Exercises - Seated - Right
Shoulder Isometric Exercises - Standing - Left
Shoulder Isometric Exercises - Standing - Right
Shoulder Passive Range of Motion - Left
Shoulder Passive Range of Motion - Right
Shoulder Pendulum Exercises - Left
Shoulder Pendulum Exercises - Right
Shoulder Prone Active Exercises - Left
Shoulder Prone Active Exercises - Right
Shoulder Prone Strengthening Exercises - Left
Shoulder Prone Strengthening Exercises - Right
Shoulder Pulley Exercises - Left
Shoulder Pulley Exercises - Right
Shoulder Resistance Band Exercises - Left
Shoulder Resistance Band Exercises - Right
Shoulder Scapular Exercises - Left
Shoulder Scapular Exercises - Right
Shoulder Stretching Exercises - Left
Shoulder Stretching Exercises - Right
Level 2 Activities - Use Your Weaker Arm to Passively Hold
Level 3 Activities - Use Your Weaker Arm to Actively Hold
Level 4 Activities - Use Your Weaker Arm with Gross Motor
Level 5 Activities - Use Your Weaker Arm with Fine Motor
Passive Range of Motion - Left Side Weakness
Passive Range of Motion - Right Side Weakness
Scapular Mobility and Strength Exercises - Left Side Weakness
Scapular Mobility and Strength Exercises - Right Side Weakness
Self Range of Motion - Left Side Weakness
Self Range of Motion - Right Side Weakness
Use Your Left Arm to Actively Move and Hold
Use Your Left Arm to Passively Hold
Use Your Left Arm with Assisted Guiding
Use Your Left Arm with Gross Motor Activities
Use Your Left Arm with Self-Guiding
Use Your Right Arm to Actively Move and Hold
Use Your Right Arm to Passively Hold
Use Your Right Arm with Assisted Guiding
Use Your Right Arm with Gross Motor Activities
Use Your Right Arm with Self-Guiding
Weight Bearing Exercises - Left Side Weakness
Weight Bearing Exercises - Right Side Weakness
Gross Motor Tasks
Median Nerve Glides
Posture Exercises
Radial Nerve Glides
Resistance Band Exercises - Arms
Ulnar Nerve Glides
Upper and Lower Body Passive Range of Motion
Upper Body Active Range of Motion
Upper Body Exercises - Dumbbells
Upper Body Exercises - Holding a Ball
Upper Body Strength Activities
O ccupational Therapy Toolkit ™
Osteoarthritis (OA), rheumatoid arthritis (RA), psoriatic arthritis (PsA)
Impairments and Functional Limitations
ADL, IADL, work and leisure impairment
Functional mobility impairment
Limited activity tolerance and endurance
Limited ROM
Impaired hand function
Impaired strength
Joint pain, swelling, and stiffness
Joint deformity and instability
Postural changes
Impaired balance
Sleep problems
Co-occurring conditions may include RA - joint deformities (swan neck, boutonniere, hitchhikers thumb, ulnar drift), nerve compression, surgery (joint replacement, joint fusion, synovectomy, tendon repair), cardiovascular disease, lung fibrosis, osteoporosis. OA - CMC arthritis, joint replacement. PsA - psoriasis, diabetes, cardiovascular disease.
Outcome Measure
Rheumatoid Arthritis Disease Activity Index (RADAI-5)
Arthritis Hand Function Test (AHFT)
Occupational Therapy Intervention
ADL, IADL, productivity and leisure training
- Train in the use of joint protection and adaptive equipment to improve grasp (built-ups), improve ease of performance (electric can opener), compensate for ROM loss (dress stick), compensate for weak/absent muscle (universal cuff, jar opener), prevent stress on joints (lever door handle), prevent prolonged grasp (book holder, Dycem), prevent accidents (bath seat, nonskid rugs).
- Instruct in body mechanics and good posture.
Train in safe and efficient functional mobility (sit-to-stand, bed mobility skills, transfers, standing, ambulation, and wheelchair mobility) during ADL and IADL tasks.
- Adaptive mobility equipment - hospital beds, lift chairs, standard/electric wheelchairs, transfer boards, hydraulic patient lifts, leg lifter, bed rails.
Provide orthotics to maintain/correct joint alignment, improve function, correct or minimize deformities/contractures, and support weak or painful joints. Examples for RA include resting hand splint, wrist cock-up splint, ulnar drift splint, anti-swan neck deformity splints (oval 8), anti-boutonniere splint. Examples for OA include CMC orthosis, thumb spica splint, DIP/PIP orthosis.
Teach strategies to self-manage fatigue and conserve energy.
- Assess using the Modified Fatigue Impact Scale.
- Teach pacing and energy conservation strategies.
- Instruct in balancing self-care, productivity, play, and rest.
- Instruct in good sleep habits.
- Encourage use of a fatigue journal.
- Problem-solve ways to self-manage fatigue.
Provide an individualized exercise program that includes low-impact, low-intensity endurance, strengthening, flexibility, and balance activities. Modify exercises (use yoga blocks, wrap foam around weights, weight lifting gloves to improve grip).
- Acute flare-ups - instruct in performing gentle passive or active ROM exercises 3-4 times daily followed by icing for 15 minutes.
- Non-acute joints - instruct in the use of superficial heat, passive or active ROM and isometric strengthening in pain free range.
- Encourage participation in community programs. (Tai Chi, Active Living Every Day, Arthritis Foundation Aquatic Program, Arthritis Foundation Exercise Program, Enhance Fitness, Fit and Strong, Walk with Ease).
Provide pain management.
- Modalities (heat, cold, ultrasound, fluidotherapy, paraffin).
- Manual therapy techniques (massage, soft tissue mobilization).
Instruct in pain self-management strategies.
- Coordinate medication peak with exercise and activity.
- Superficial heat, cool/cold water, contrast baths.
- Self-massage techniques (foam rollers, tennis ball, rolling massage stick).
- Breathing techniques, mindful meditation or other relaxation methods.
- Positioning devices (seat cushions, back supports, pillows, splints).
- Encourage use of a pain journal.
- Problem-solve ways to self-manage pain.
Complete a comprehensive, performance-based home and/or work assessment. Recommend and/or provide modifications, accommodations, adaptive equipment, and/or assistive technology.
Provide education about fall risk and prevention strategies.
Teach strategies to incorporate wellness and health management routines into daily activities.
Educate patient and caregivers about arthritis, the availability of community resources and support groups.
Patient and Caregiver Handouts
Body Mechanics - Good Posture
Exercise Tips for Arthritis
Finger and Thumb Stretches and Active Range of Motion
Forearm and Wrist Active Range of Motion
Forearm and Wrist Stretches
Joint Protection for Arthritis
Pain Journal
Putty Exercises
Shoulder Isometric Exercises - Seated
Splint/Brace Instructions
Stress Management
Tendon Glides
Tips to Conserve Energy
Upper Body Active Range of Motion
Using Cold for Pain Relief
Using Heat for Pain Relief
Additional Treatment Guides
Ankylosing Spondylitis
Carpal Tunnel Syndrome
Cubital Tunnel Syndrome
Health Management
Joint Contractures
Lupus (Systemic Lupus Erythematosus)
Rest and Sleep
Scleroderma (Systemic Sclerosis)
Sexual Expression and Activity
Total Hip Replacement (Arthoplasty)
Total Knee Replacement (Arthoplasty)
Total Shoulder Arthroplasty and Hemiarthroplasty
Work and Industry
O ccupational Therapy Toolkit ™
Pre and Postoperative Management
Impairments and Functional Limitations
ADL, IADL, productivity and leisure impairment
Impaired ROM and strength of trunk and upper extremity
Post-op pain and edema
Potential secondary complications may include nerve damage, lymphedema
Assessments
Disabilities of the Arm, Shoulder, and Hand Questionnaire
Functional Assessment of Cancer Therapy - Breast
Occupational Therapy Preoperative Intervention
- Baseline measurements (ROM, strength, sensation, and limb volume measurements, functional outcome measure such as DASH))
- Provide education about postoperative activity limitations, precautions and exercise.
- Instruct in good posture during activities.
- Educate about lymphedema prevention or risk factor reduction.
- Teach strategies to incorporate wellness and health management routines into daily activities.
- Educate about breast cancer and the availability of community resources. Encourage participation in support groups.
Occupational Therapy Postoperative Intervention
ADL, IADL, productivity and leisure training
- Treat underlying limitations to safety and independence.
- Recommend and/or provide adaptive equipment as needed. Train in lower body ADL equipment following reconstructive surgery involving abdominal muscles.
- Instruct in good posture during activities.
- Instruct to elevate arm several times a day to self-manage postoperative edema.
- Instruct in protective use of affected arm for the first 2 weeks. Unless otherwise instructed by surgeon.
- Avoid overuse.
- Avoid sleeping on the same side as the surgery.
- Avoid lifting more than 5 lbs./2.25 kg.
- Keep tasks below 90° of shoulder motion.
Train in safe and efficient functional mobility (sit to stand, bed mobility skills, transfers, ambulation and wheelchair mobility) during ADL and IADL tasks.
Pain self-management
- Coordinate medication peak with exercise and activity.
- Teach stress management and relaxation techniques.
- Use pillows to help the arm and shoulder relax while sitting and lying down.
- Instruct in good posture during activities.
Provide graded UE activities and exercises. Follow the referring surgeon’s specific guidelines for ROM and progression of exercises.
- AROM exercises within restricted ranges according to surgical intervention. Progress exercises until full ROM restored. Begin strengthening 4-6 weeks after surgery.
- Instruct in deep (diaphragmatic) breathing exercises and lateral expansion.
- Instruct in a walking program.
Provide surgical scar management. Treat axillary web syndrome if present.
Educate about lymphedema prevention or risk factor reduction. Manage lymphedema using Complete Decongestive Therapy (CDT) (performed by a certified lymphedema therapist).
Patient and Caregiver Handouts
Arm Measurement
Body Mechanics - Good Posture
Deep (Diaphragmatic) Breathing
Edema (Swelling) Control of the Arm(s)
Mastectomy Exercises
Median Nerve Glides
Radial Nerve Glides
Scar Massage
Tips to Prevent Upper Body Lymphedema
Ulnar Nerve Glides
Walking Guidelines
Additional Treatment Guides
Cancer
Health Management
Lymphedema
O ccupational Therapy Toolkit ™
Dressing includes selecting appropriate clothing for the time of day, weather, and occasion. Obtaining clothing from closets and drawers. Dressing and undressing using open-front garments (shirt/blouse, robe, sweater, jacket, winter coat), pullover garments (sweatshirt, t-shirt, sweater), bra, pants, skirts, suspenders, necktie, scarf, gloves, underwear, socks, pantyhose, nylons, shoes, boots, slippers, support and anti-embolism stockings. Opening and closing fasteners, (snaps, buttons, hooks, zippers, Velcro). Managing personal medical devices (hearing aids, eyeglasses, contacts, AFO, hand splint, back brace, slings, and prosthetics).
Occupational Therapy Intervention
Apply different approaches for solving difficulties with dressing.
- Remediate underlying limitations to safety and independence. Physical (e.g. muscle weakness, limited ROM, fatigue), sensory (e.g. impaired sensation, low vision, pain), behavioral (e.g. anxiety, depression, impulsivity), cognitive (e.g. impaired attention, memory, language and communication, or executive functions), perceptual (e.g. unilateral neglect, impaired figure ground).
- Train in compensatory techniques (safety techniques, one-handed techniques, pacing, energy conservation, joint protection, body mechanics, breathing techniques, low vision techniques, cognitive/perceptual compensation, step-by-step instructions, task segmentation, task sequencing, backward chaining, verbal and physical cueing, hand-over-hand guiding).
- Train in the use of adaptive equipment and assistive devices (buttonhook, Velcro closures on shoes, elastic shoelaces, long handled shoehorn, dressing stick, reacher, sock aid, zipper pull, loops on pants, loops on socks, labeling system for identifying clothes, and specialized clothing).
- Provide environmental modifications and adaptations (avoid storing items on the floor, lower closet poles, organize clothes within easy reach, and label drawers using picture or words).
- Instruct in activity modification.
- Change the task (place the weaker extremity into the garment first, dress in a supine position).
- Eliminate part or all of the task (choose garments that are easy to put on and remove such as: elastic waist pants, loose fitting tops, pullover tops, suspenders instead of a belt, Velcro shoes, slip on shoes, front hook bra, sports bra, camisole).
- Have someone else do part or the entire task.
Train in safe and efficient functional mobility (sit to stand, bed mobility skills, transfers, standing, ambulation, and wheelchair mobility) during dressing tasks.
Provide caregiver/family education and training.
Patient and Caregiver Handouts
Dressing Tips
Tips to Conserve Energy with Self Care Tasks
Dressing Techniques - Lower Body
Put On and Take Off an Ankle-Foot Brace - Method 1 - Right Leg
Put On and Take Off an Ankle-Foot Brace - Method 2 - Left Leg
Put On and Take Off an Ankle-Foot Brace - Method 2 - Right Leg
Put On and Take Off Pants - Method 1
Put On and Take Off Pants - Method 2
Put On and Take Off Pants, Socks, and Shoes Lying Down
Put On and Take Off Pants, Socks, and Shoes Using a Stool
Put On and Take Off Pants Using a Dressing Stick or Reacher
Put On and Take Off Socks and Shoes Using Dressing Tools
Put On and Take Off Support Stockings
Dressing Techniques - One Handed
Put On a T-shirt with One Hand - Right Side Weakness
Put On an Open Front Shirt with One Hand - Left Side Weakness
Put On an Open Front Shirt with One Hand - Right Side Weakness
Put On and Take Off a Bra with One Hand - Left Side Weakness
Put On and Take Off a Bra with One Hand - Right Side Weakness
Put On Pants with One Hand - Left Side Weakness
Put On Pants with One Hand - Right Side Weakness
Put On Socks and Shoes with One Hand - Left Side Weakness
Put On Socks and Shoes with One Hand - Right Side Weakness
Take Off a T-shirt with One Hand - Left Side Weakness
Take Off a T-shirt with One Hand - Right Side Weakness
Take Off an Open Front Shirt One Hand - Left Side Weakness
Take Off an Open Front Shirt One Hand - Right Side Weakness
Take Off Pants with One Hand - Left Side Weakness
Take Off Pants with One Hand - Right Side Weakness
Tie Shoes with One Hand - Left Side Weakness
Tie Shoes with One Hand - Right Side Weakness
Dressing Techniques - Upper Body
Put On and Take Off a T-shirt - Head-Arm-Arm
Put On and Take Off a T-shirt Using a Dressing Stick
Put On and Take Off an Open Front Shirt - One Shoulder Drape
Put On and Take Off an Open Front Shirt - Two Shoulder Drape
Put On and Take Off an Open Front Shirt Using a Dressing Stick
Using a Buttonhook
O ccupational Therapy Toolkit ™
Impairments and Functional Limitations
ADL, IADL, productivity and leisure impairment
Functional mobility impairment
Slow walking speed
Muscle weakness
Limited activity tolerance and endurance
Impaired balance
Impaired vision and hearing
Chronic pain
At high risk for major adverse health outcomes including institutionalization, disability, falls, hospitalization, and mortality
Co-occurring conditions may include functional decline, falls, fear of falling, delirium, dementia, dizziness, depression, incontinence, sleep disorders, malnutrition, dehydration, pressure ulcers, sarcopenia, hypothermia, hyperthermia
Assessments
Edmonton Frail Scale
FRAIL (Fatigue, Resistance, Aerobic capacity, Illnesses, Loss of weight) Scale
Groningen Frailty Index
Johns Hopkins Frailty Assessment Calculator
SHARE-FI (Survey of Health, Ageing and Retirement in Europe Frailty Index)
Occupational Therapy Intervention
ADL, IADL, productivity and leisure training
- Treat underlying limitations to safety and independence - physical (strength, hand function, ROM, coordination, balance, endurance, abnormal tone), sensory (tactile, vision, hearing, vestibular, pain), behavioral, cognition and/or perceptual.
- Address nutrition - oral health, ability to feed self, ability to shop, access kitchen, prepare nutritious meals and get adequate hydration. Encourage to eat with others.
- Address ability to drive safely. Provide referral to driving rehab specialist and/or explore alternative transportation options.
Train in safe and efficient functional mobility (sit to stand, bed mobility skills, transfers, standing, ambulation and wheelchair mobility) during ADL and IADL tasks.
- Train in the safe and correct use of assistive devices and adaptive equipment (walkers, canes, sliding boards, bed transfer handles, leg lifters, wheelchairs) as appropriate.
Provide an individualized exercise program that includes progressive endurance, strengthening and flexibility activities.
Instruct patient and caregiver in a written home exercise program.
Provide functional balance activities to increase balance confidence with ADL tasks.
Provide pain management.
Provide a fall prevention program that includes balance, coordination, and agility training, and education about fall risk and prevention strategies. Provide functional balance activities to increase balance confidence with ADL tasks.
Complete a comprehensive, performance-based home assessment. Recommend and/or provide modifications, adaptive equipment and/or assistive technology.
Educate about the negative effects of prolonged sitting and bed rest. Educate regarding hypothermia and hyperthermia prevention.
Patient and Caregiver Handouts
Balance Exercise
Hip and Knee Exercises - Seated
Putty Exercises
Resistance Band Exercises - Arms
Resistance Band Exercises - Legs
Upper Body Exercises - Dumbells
Walking Guidelines
Additional Treatment Guides
Balance
Chronic Pain Syndrome
Fall Risk Assessment and Prevention
Functional Mobility
Health Management
Home Safety and Modification
Pressure Ulcers
Rest and Sleep
Urinary Incontinence
O ccupational Therapy Toolkit ™
Impairments and Functional Limitations
ADL, IADL, productivity and leisure impairment
Impaired functional mobility
Hemiparesis or hemiplegia of the upper and lower extremities
Spasticity
Impaired postural control and balance
Impaired coordination
Limited activity tolerance and endurance
Impaired sensation
Central post-stroke pain
Language disorders (aphasia, dysarthria, dyspraxia)
Dysphasia
Visual and perceptual impairment
Cognitive impairment
Behavioral disorders (depression, lability, low frustration tolerance, impulsivity)
Bladder and bowel dysfunction
Potential secondary complications may include biomechanical shoulder pain (biceps tendonitis, rotator cuff pathology, adhesive capsulitis, complex regional pain syndrome), edema (upper and lower extremity), pressure ulcers, joint contractures, depression, DVT’s, aspiration pneumonia, seizures, fall risk
Assessments
Assessment of Motor and Process Skills
Chedoke-McMaster Stroke Assessment Scale
Modified Ashworth Scale of Spasticity
Stroke Impact Scale
Occupational Therapy Intervention
ADL, IADL, productivity and leisure training
- Safely incorporate affected extremity with all activities.
- Use compensatory techniques (task modification, one-handed techniques, hand-over-hand guiding, task segmentation, backward chaining).
- Recommend and/or provide adaptive equipment. Rocker knife, inner lip plates, holders for books or playing cards, stabilizing devices for activities that traditionally require two-handed performance (cutting vegetables, cleaning dentures), and keyboards adapted for one-handed computer use.
- Instruct in pacing and energy conservation strategies.
Train in safe and efficient functional mobility (sit-to-stand, bed mobility skills, transfers, standing, ambulation, and wheelchair mobility) during ADL and IADL tasks.
Provide functional posture and balance activities.
- Focus on stability, weight shifting, body awareness, trunk rotation & elongation.
- Have patient turn toward affected side when reaching.
- Set up room so the patient must physically move to their affected side.
- Provide reach-grasp-hold-release activities, in standing and sitting, with and without support.
Provide activities and exercises to uninvolved side to prevent loss of ROM and strength.
Restore function of the upper extremity. Use a variety of remedial approaches according to the needs of the patient.
- Provide early mobilization and positioning.
- Incorporate task-oriented/task specific training.
- Provide opportunities to use and move the arm throughout the day (use of mobile arm support, overhead suspension sling, functional splinting such as wrist cock-up, and dynamic finger extension splints).
- Provide modified constraint-induced movement therapy or constraint-induced movement therapy.
- Instruct an arm and hand strengthening exercise program.
- Cyclic NMES during functional movements and activity.
- Instruct in a functional dynamic orthoses (SaeboFlex, SaeboReach).
- Use cognitive strategies (mirror therapy, mental imagery/practice, action observation).
- Provide sensory re-education intervention.
- Avoid increasing spasticity.
- Encourage use of extremity in functional tasks.
- Provide weight-bearing activities.
- Provide sensory stimulation activities.
- Teach compensatory techniques and safety measures for sensory deficits. Use vision to compensate for sensory loss. Test bath/dish water temperature using the intact extremity or a thermometer. Use a thermal regulation valve to lower water temperature. Avoid using heating pads on impaired extremities. Wear gloves to prevent frostbite. Avoid going barefoot. Wear sunscreen to prevent sunburn. Avoid cuts and burns in kitchen. Use intact hand to handle sharp kitchen utensils. Perform skin checks.
- Prevent or manage hand edema.
- Teach active self-range of motion exercises in elevation.
- Position hand in elevation
- Use retrograde massage.
- Use gentle grade 1-2 mobilizations for the hand and fingers.
- Provide a compression garment.
- Manage spasticity.
- Prevent contractures.
- Provide PROM, SROM and stretching exercises.
- Instruct in positioning in bed, chair and during mobility.
- Select use of splinting to protect hand/wrist. Resting hand splint for flaccid to mild tone, spasticity splint for moderate to high tone. Reassess frequently and discontinue of there is no benefit.
- Post-Botox injections, provide strengthening/FES to antagonists, stretching and splinting
- Prevent or manage shoulder pain.
- Avoid overaggressive therapy and overhead pulleys.
- Mobilize and strengthen the scapula.
- Position arm with cubital fossa facing up, 45º shoulder abduction and comfortable shoulder external rotation.
- Provide firm support devices such as lap trays and arm troughs.
- Range of motion exercises should not move the shoulder beyond 90°of flexion and abduction unless there is upward rotation of the scapula and external rotation of the humeral head.li>
- o Manage acquired orthopedic conditions (biceps tendonitis, impingement syndrome, adhesive capsulitis, rotator cuff pathologies, CRPS).
- Use functional electrical stimulation (FES) for shoulder subluxation.
Instruct patient and caregivers in care of the affected extremity.
- Prevent and control of edema.
- Teach passive ROM exercises.
- Teach self-ROM exercises.
- Protect and support the affected arm during bed mobility, transfers and ambulation using slings, a pocket, or hand hold and during wheelchair use by using a hemi tray or arm trough.
- Teach proper positioning in bed, chair and wheelchair.
- Instruct in care and use of positioning splints.
Teach compensatory strategies for perceptual deficits.
Provide cognitive retraining and train in the use of compensatory strategies.
Provide education about fall risk and prevention strategies.
Community reintegration
- Complete a comprehensive, performance-based home assessment. Recommend and/or provide modifications, adaptive equipment and/or assistive technology.
- Encourage leisure and social participation.
- Address ability to drive safely. Provide referral to driving rehab specialist and/or explore alternative transportation options.
- Recommend vocational rehabilitation strategies to assist with return to work if appropriate.
Teach strategies to incorporate wellness and health management routines into daily activities.
Educate patient and caregivers about stroke, the availability of community resources. and support groups. Provide educational materials about stress management, coping strategies, and occupational balance.
Patient and Caregiver Education Handouts
Edema (Swelling) Control of the Arm(s)
Edema (Swelling) Control of the Leg(s)
In and Out of Bed - Toward Your Weaker Left Side
In and Out of Bed - Toward Your Weaker Right Side
Position in Bed - Left Side Weakness
Position in Bed - Right Side Weakness
Position Your Arm - Left Side Weakness
Position Your Arm - Right Side Weakness
Protect the Arm - Left Side Weakness
Protect the Arm - Right Side Weakness
Splint/Brace Instructions
Stress Management
Tips to Conserve Energy
Using a Front Wheel Walker (2 wheels)
Wheelchair Safety
Patient and Caregiver Exercise Handouts
Balance Exercises - Sitting and Standing
Fine Motor Strengthening and Coordination Activities
Gross Motor Tasks
Level 1 Activities - Help Your Weaker Arm Move
Level 2 Activities - Use Your Weaker Arm to Passively Hold
Level 3 Activities - Use Your Weaker Arm to Actively Move and Hold
Level 4 Activities - Use Your Weaker Arm with Gross Motor
Level 5 Activities - Use Your Weaker Arm with Fine Motor
Passive Range of Motion - One Side Weakness
Posture Exercises
Putty Exercises
Scapular Mobility and Strength Exercises
Self Range of Motion
Upper Body Active Range of Motion
Upper Body Exercises - Dumbbells
Upper Body Exercises - Holding a Ball
Upper Body Strength Activities
Use Your Arm to Actively Move and Hold
Use Your Arm to Hold Passively
Use Your Arm with Assisted Guiding
Use Your Arm with Gross Motor Activities
Use Your Arm with Self-Guiding
Weight Bearing Exercises
Additional Treatment Guides
Activities of Daily Living
Apraxia
Balance
Cognition
Depression
Fall Risk Assessment and Prevention
Functional Mobility
Handwriting
Health Management
Home Safety and Modification
Therapeutic Exercise
Visual Skills
Wheelchair Seating, Positioning, and Mobility
O ccupational Therapy Toolkit ™
Left Side Weakness

Step 1
Place the shirt face down on your lap with the collar at your knees.

Step 2
Gather the hole of the left sleeve and place on your lap.

Step 3
Lean forward and place your left arm into the sleeve hole.

Step 4
Pull the sleeve up your arm and over your elbow.

Step 5
Place your right arm into the right sleeve hole.

Step 6
Grasp the shirt and pull it over your head.

Step 7
Push the shirt over your left shoulder.

Step 8
Adjust the shirt, by pulling it down in the front and the back.
O ccupational Therapy Toolkit ™
Do the checked exercises _____ times per day, _____ days a week

- Shape the putty into a ball. Squeeze the putty with all your fingers.
Do _____ sets of _____.

- Shape the putty into a ball. Hold the putty in your hand. Press your thumb into the putty.
Do _____ sets of _____.

- Shape the putty into a ball. Pinch the putty between your thumb and the side of your index finger.
Do _____ sets of _____.

- Shape the putty into a ball. Hold your fingers straight and your knuckles bent. Squeeze the putty between your fingers and thumb.
Do _____ sets of _____.

- Flatten the putty into a pancake. Place your fingers into the center of the putty and spread the putty outward.
Do _____ sets of _____.

- Flatten the putty into a pancake. Spread the putty apart using two fingers at a time.
Do _____ sets of _____.

- Shape the putty into a sausage. Squeeze the putty between your fingers.
Do _____ sets of _____.

- Shape the putty into a sausage. Pinch the putty between your thumb and each finger.
Do _____ sets of _____.
O ccupational Therapy Toolkit ™
Pace yourself, rest often, and use pursed lip breathing.
Eating
- Eat slowly and fully chew food.
- Eat six small meals a day instead of three big meals.
- Do not eat gas-forming food. They can bloat your stomach and make it harder to breathe. These include peas, melons, turnips, onions, cauliflower, apples, corn, broccoli, cucumbers, cabbage, beans, and Brussels sprouts.
Grooming
- Sit to shave, comb your hair and brush your teeth.
- Support your elbows on the counter while grooming or shaving.
- Use an electric toothbrush and an electric razor.
- Wash your hair in the shower. Keep your elbows low and your chin tucked.
Bathing and Showering
- If you use oxygen during exercise, then use it when you take a shower.
- Allow plenty of time.
- Gather all the items you will need.
- Sit to bathe and dry. Use a bath chair in the shower.
- Limit bending. Use a long brush to wash your back and feet. Use a hand-held shower to rinse.
- Use a shower caddy and soap on a rope. Place soap in a nylon stocking tied to the shower seat or soap dish.
- Dry off using hand towels because they are not as heavy. Put on a terry cloth robe to dry off.
Dressing
- Allow plenty of time.
- Gather all the items you will need.
- Sit to dress and undress.
- Limit bending. Put your foot on your other knee or use long-handled tools to put on pants, shoes and socks.
- Wear clothes that are easy to put on. Try slip-on shoes, stretch waistbands, and one size larger.
- Do not wear tight clothes like belts, ties, tight socks, girdles and bras.
O ccupational Therapy Toolkit ™

1. Face the wall and hold onto the grab bar.

2. Step into the tub with your left leg.

3. Lift your right leg into the tub.
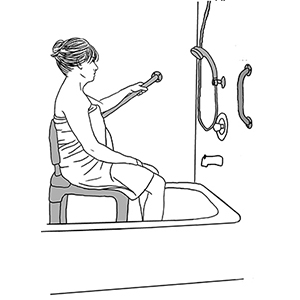
4. Sit down on the shower chair.
Reverse
the steps to get out.
O ccupational Therapy Toolkit ™
Use your left arm as much as you can during the day. Here are a few ideas.

Use your left hand to hold your plate while eating.

Hold a sheet of paper with your left hand while writing with your right hand.

Hold a wash cloth with your left hand and apply soap with your right hand.

Hold your toothbrush with your left hand and apply toothpaste with your right hand.
O ccupational Therapy Toolkit ™
Usando el Método de Una Mano - Lado Izquierdo Afectado

Paso 1
Posicione su camiseta boca abajo en su regazo con el cuello de la camisa en las rodillas.

Paso 2
Agarre la apertura de la manga izquierda y colóquela en su regazo.

Paso 3
Inclínese hacia adelante y coloque el brazo izquierdo en la apertura de la manga.

Paso 4
Suba la manga sobre el brazo y sobre el codo.

Paso 5
Coloque el brazo derecho en la apertura de la manga derecha.

Paso 6
Agarre el tejido y tire de la camiseta sobre su cabeza.

Paso 7
Empuje el tejido de la camiseta sobre el hombro izquierdo.

Paso 8
Ajuste la camiseta, tirando de ella hacia abajo por delante y por detrás.
O ccupational Therapy Toolkit ™
Haga los ejercicios marcados _____ veces al día, _____ días a la semana.

- Moldee la masilla en forma de pelota. Apriete la masilla con su mano completa.
Complete _____ series de _____.

- Moldee la masilla en forma de pelota. Agarre la masilla con la mano. Presione con el pulgar hacia el interior de la masilla.
Complete _____ series de _____.

- Es la que emplearía para usar una llave. Moldee la masilla en forma de pelota. Pellizque la masilla entre el pulgar y el lateral del dedo índice.
Complete _____ series de _____.

- Moldee la masilla en forma de pelota.Estire los dedos y doble los nudillos. Apriete la masilla entre sus dedos y pulgar.
Complete _____ series de _____.

- Aplane la masilla en forma de tortita. Coloque la punta de los dedos juntos en la masilla, y expanda la masilla hacia fuera.
Complete _____ series de _____.

- Aplane la masilla en forma de tortita. Expanda la masilla usando dos dedos a la vez.
Complete _____ series de _____.

- Moldee la masilla en forma de salchicha. Apriete la masilla entre los dedos.
Complete _____ series de _____.

(punta con punta)
- Moldee la masilla en forma de salchicha. Pellizque la masilla entre el pulgar y cada uno de los dedos individualmente.
Complete _____ series de _____.
O ccupational Therapy Toolkit ™
Comer
- Coma seis comidas pequeñas al día en lugar de tres comidas grandes. Esto disminuye la energía necesaria para comer y digerir la comida.
- Coma lentamente y mastique completamente la comida.
- Evite comidas que produzcan gases, lo que puede hinchar el abdomen y dificultar la respiración, como guisantes, melones, nabos, cebollas, coliflores, manzanas, maíz, brócoli, pepinos, repollos, judías, y coles de Bruselas.
Aseo
- Siéntese para afeitarse, peinarse y lavarse los dientes
- Apoyo sus codos en una superficie mientras se arregla o se afeita.
- Use un cepillo de dientes eléctrico y una máquina de afeitar eléctrica.
- Lávese el pelo en la ducha. Mantenga los codos bajos y la barbilla hacia abajo.
Bañarse y Darse una Ducha
- Si su doctor le ha prescrito oxígeno para usarlo durante el ejercicio, úselo cuando se dé una ducha.
- Reúna todos los artículos que necesitará, incluyendo la ropa.
- Siéntese para quitarse la ropa, bañarse, secarse y vestirse. Use una silla de baño en la ducha.
- Evite estirarse demasiado. Use una esponja con mango largo para lavarse la espalda y los pies. Use una alcachofa de ducha de mano para enjuagarse.
- Use una estantería para la ducha y una pastilla de jabón con cuerda, o coloque el jabón en una media de nylon y átela a la silla de ducha o jabonera.
- Tenga una toalla o albornoz cerca. Considere usar toallas de mano pues no son tan pesadas. Póngase una bata de felpa para evitar la necesidad de secarse.
Vestirse
- Antes de comenzar, reúna toda la ropa, zapatos, etc.
- Siéntese para vestirse.
- Evite inclinarse cruzando una pierna sobre la otra, use un taburete o equipo adaptado con mangos alargados para ponerse pantalones, zapatos y calcetines.
- Lleve calzado fácil de poner, cómodo y sin cordones; use un calzador de mango alargado. Use cinturas elásticas y camisas una talla más grande.
- Evite la ropa restrictiva, como las medias apretadas, las fajas, y sujetadores. Use tirantes si los cinturones son demasiado restrictivos.
O ccupational Therapy Toolkit ™
(pierna izquierda, derecha, sentarse)

Paso 1
Mirando a la pared, agarre el asidero.

Paso 2
Entre en la bañera con su pierna izquierda

Paso 3
Levante su pierna derecha hasta entrar en la bañera.
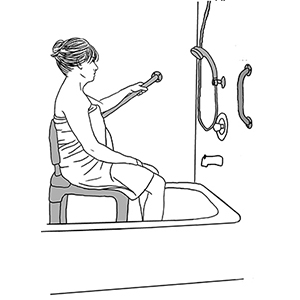
Paso 4
Siéntese en la silla de ducha. Invierta los pasos para salir de la bañera.
O ccupational Therapy Toolkit ™
Es muy importante que utilice el brazo afectado todo lo posible durante las actividades diarias. Aquí hay algunos ejemplos sobre cómo puede hacerlo.

Use la mano izquierda para estabilizar el plato mientras come.

Estabilice una hoja de papel con la mano izquierda mientras escribe con la derecha.

Estabilice el paño con la mano izquierda mientras aplica jabón con la mano derecha.

Estabilice el cepillo de dientes con la mano izquierda mientras usa la derecha para aplicar pasta de dientes.
